Histological Features (Histology) (For professionals)
Seborrhoeic keratosis=SK
In case of diagnostic doubt, a shave biopsy ought to be done. SK are benign epithelial tumours which are part of the group of acanthomas {Brownstein, 1985}. SK is postulated to be of follicular keratinocytic origin {Mehregan, 1964; Degos, 1968}, and can show an exophytic (upwards) sometimes endophytic (downwards)(ie. IFK) pattern of growth {Wade, 1979}.
1. Common features
Different histological types of SK have been recognized but all have characteristics in common:
A. Epidermis
Structurally, in contrast with normal skin, varying degrees of acanthosis, hyperkeratosis, focal hypergranulosis and papillomatosis {Kao, 2000}are found. The abrupt transition between the normal and SK epidermis is called the string sign {Pierson, 2003}.No cellular atypia {Pierson, 2003}, nor parakeratosis{Korting, 1976} are present, with the exception of some irritated types of SKs.
Two types of cells are found: basaloid and squamous-like cells. Squamous-like cells have the appearance of keratinocytes found in the stratum spinosum of normal skin{Kirkham, 1997}. Basaloid cells are small and uniform in aspect with a relatively voluminous and hyperchromatic nucleus compared with little cytoplasm, as in the stratum basale in normal skin{Kirkham, 1997}. In edematous areas, intercellular bridges can be seen {Andrade, 1959}.
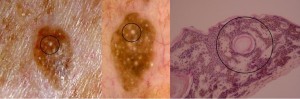
Invaginations of the epidermis filled with keratin called pseudohorn cysts (comedo-like cysts on dermoscopy) on dermoscopy)are characteristic of these lesions. The term “horn cysts” (milia-like cysts on dermoscopy), contrarily to pseudohorn cyts do not communicate with the surface. Let us underline that cysts tend to be over estimated and pseudohorn cysts underestimated due to the histological sections which are two dimensional.
Melanin distribution is not always limited to basal keratinocytes. It is usually found in parallel with basaloid cell proliferation {Mishima, 1960}, melanophagic cells, are heavily present in the papillary dermis in deeply pigmented lesions.
In 18% of SKs {Olsen, 1994} an amyloïd deposit is present.
B. Dermo-epidermal junction
{Pierson, 2003}The base of SKs are devoid of epidermal or dermal papillae, and thus appears more or less as a horizontal line.
C. Dermis
A stromal reaction is not generally found, excepting in the acanthotic {Kao, 2000} and irritated{Korting, 1976} types of SK.
2. Histological types
Even though SK lesions have characteristics in common, at least 5 types {Habif, 2001}have been recognized. The first three subtypes are much more frequent than the latter two. A single lesion can contain different types{Habif, 2001}. As a summary, reticulate types are always acanthotic and can be grouped together. A slide with a prominent stratum corneum can be labelled as Acanthohyperkeratotic. Both regrouped types can show a variable degree of irritation and pigmentation. Clonal SKs and IFKs are considered separately because they appear less frequently.
A. Acanthotic
It is the most frequent type {Kirkham, 1997}. It presents clinically as a non keratotic dome-shaped papule even though no proof of a clinical-histological correlation exists{Pierson, 2003}.
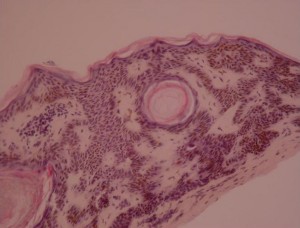
The acanthotic {Kirkham, 1997}sometimes pigmented epidermis consists of columns of basaloid cells with pseudohorn cysts and horn cysts in between {Wade, 1979}.
This type often contains an amount of pigment superior in quantity than others. Indeed, one third of slides stained with hematoxylin-eosin {Becker, 1951} and two thirds of slides stained with silver {Lennox, 1949} contains an excess of melanin. As for the distribution of melanin, it is generally basally located, but all layers can be pigmented, and that in parallel with basaloid cell proliferation {Mishima, 1960}.
As for the dermis, inflammation characterized by a lymphomononuclear infiltrate is frequently present {Kao, 2000}. Melanophagic cells, are present in the papillary dermis proportionally with the quantity of pigment present{Kao, 2000}.
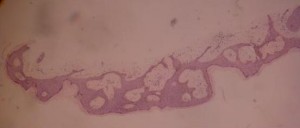
B. Reticulate (or adenoidal)
The epidermis is characterised by a thin strand of basaloid cells which extend from the follicular keratinocytes and intermingle with each other {Wade, 1979}. This type often displays focal areas of hyperkeratosis, areas where pseudocysts and horn cysts are to be found{Kirkham, 1997}.
It has been postulated that this type of KS has a close relationship with solar (senile) lentigo {Mehregan, 1975}(see causal factors).
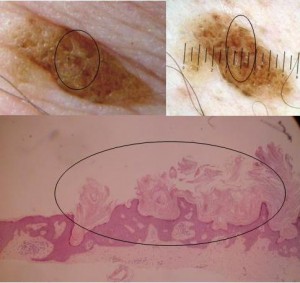
C. Hyperkeratotic (AHCS) {Pierson, 2003}
Also called papillomatous, or digitate, or serrated SK, this type is histologically opposed to the acanthotic type.
In the epidermis, hyperkeratotic SKs can display acanthosis, but are characterised by an important papillomatosis and hyperkeratosis. The epidermal keratinocyte projections towards the stratum corneum have a church-spire appearance.
Squamous like cells are more numerous than basaloid cells. Abundant pigmentation is typically absent. Pseudocysts rarely keratinize.
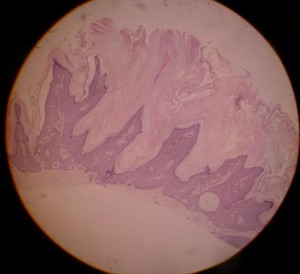
Acanthohyperkeratotic type of SK: the sharp projections adjoining the stratum corneum are called church spires
D. Clonal
This rarer subtype is characterised by nests of “basaloid” cells, which ressembles the Borst Jadassohn phenomenon, which is found in spinocellular carcinoma in situ {Wade, 1979}. The “basaloid” cells have a monomorphous and dense nuclei, and don’t have detectable desmosomes{Kao, 2000} Despite these peculiar cells, there is no cellular pleiomorphism, excessive mitosis or atypia {Kao, 2000}.
E. Irritated (activated)
{Wade, 1979} The epidermis contains epidermal nests called squamous eddies{Pierson, 2003}. The cells are intensely eosinophilic and are disposed in an onion peel fashion {Kao, 2000}. Indeed, this reaction would represent an immunological reaction{Berman, 1980; Berman, 1982} against SK lesions which leads the basaloid cells to convert into squamous-like cells. Squamous eddies, as well as the basal part of SKs, contain apoptotic cells Pesce, 2000}.The keratinocytes in the squamous eddies (or elsewhere?) are increased in size {Pesce, 2000}. Discrete to moderate atypia and mitotic cells, in contrast with other types may be present.
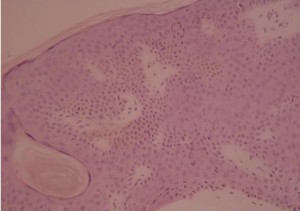
F. Inverted follicular keratosis (follicular poroma, basosquamous cell acanthoma)
This belongs to the irritated SK subtype. It shows contrary to “classical” irritated SK an endophytic pattern of growth.
{Pierson, 2003}Histologically it resembles irritated SK. Squamous eddies are present, but they sometimes keratinize in their center. What is different, is that there is a bulb like endophytic proliferation of eosinophilic keratinocytes, which have a basaloid or squamous-like morphology. The lesion is bordered by basaloid cells arranged in a palissade manner.
H. A skin disease sometimes considered as a variant of SK: Melanoacanthoma
{Pierson, 2003}Originally described by Bloch and then named type 1 non nevoid epithelioma {Mishima, 1960}, this type shows dendritic melanocytes packed with melanin {Simon, 1991}, which is absent in keratinocytes. This is probably due to a lack of transfer of melanin, although the mechanism is unknown {Tomich, 1990}.
Differential diagnosis on histology. Utility of histological analysis
Histological diagnosis is always helpful in case of a diagnostic doubt. The localisation of the lesion is invaluable, often diminishing the differential diagnosis to one or two. Because of the changing features within a SK, the whole lesion should be excised and sent to histology. This also renders a missed diagnosis of basal cell carcinoma much less possible (collision theory).
The differential diagnosis with remarks is:
A. Papillomatous lesions
B. Acanthosis nigricans
Localisation: – body folds
C. Epidermal naevus
They have a different clinical presentation. Even though they may resemble SKs, they are present at birth or early childhood and have a linear or whorled disposition. Contrarily to SKs, a hair shaft often comes out from them.
D. Confluent papillomatosis of Gougerot and Carteaud
These lesions have a totally different clinical presentation.
E. Acrochordons
localisation
– neck
– eyebrows
– armpits
– inguinal folds
– inframammary folds SKs localised here tend to be acanthotic, little keratosis being present. They aren’t pediculated.
F. Eccrine poroma (EP)
localisation:
– glabrous skin of the palms and soles
– scalp
The differentiation clinically evident principally from the localisation, moreover the elementary lesion is characteristic (in eccrine poroma): red friable papules arranged in pediculated and multilobular plaques. The lesion is surrounded by a moat.
Histologically, SK can be difficult to dediffentiate. EP is composed of monomorphous looking poroid basophilic cells. The cells communicate with the surface epithelium and the stroma has a delicate fibrovascular aspect. Contrarily to SK, a ductal lumen with eosinophilic cuticules is characteristic of EP. The cuticles show a positive PAS (periodic acid schiff) coloration and are resistant to diastase.
Contrarily to SKs, these lesions have malignant potential and can (rarely) transform into porocarcinomas.
G. Nevoid Hyperkeratosis of the Nipple
This rare isolated finding shows a verrucous thickening of the nipple and resembles histologically irritated SK.
Correlations between clinical findings and histology
SK have a wide range of presentation. Clinically lesions of SK seem to evolve from clinically smooth lesions to crusty ones. In our experience detailed in the etiology section, not all smooth lesions evolve and even big keratotic lesions can continue to grow.
Reticulate type of SK are by definition Acanthotic and acanthotic SK are often reticulate. That is why we considered the Acanthotic and Reticulate type of SK as a same category (RA) and the Acantho-hyperkeratotic SK as another (AHCS).
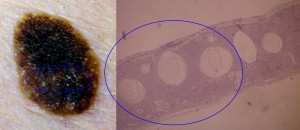
Reticulo-acanthotic type of SK (RA): Most Sks are like this and show an acanthosis af the epidermis and a reticulate pattern. From the appearance point of view, the reticulate strands of SK keratinocytes thicken so as to be later completely acanthotic. Most SKs are in between the reticulate and acanthotic extremes and show a mix of both histological subtypes.
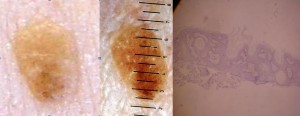
What we tried to do is to correlate clinical lesions with their histological lesions. We photographed lesions suggestive of SK and shaved them for histological confirmation.
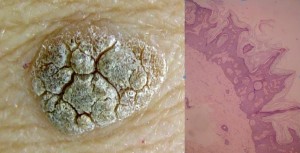
Ruguous surface are more evolutive SK with a histological diagnosis of Acanthohyperkeratotic type (AHCS). This corresponds to a thick stratum corneum.
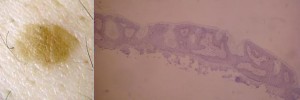
Smooth appearing young SK with a histological diagnosis in the Reticulo-acanthosic type (RA). This corresponds to a thin stratum corneum.
Clinically smooth lesions were of the reticulate and/or acanthotic type and keratotic lesions were of the acanthohyperkeratotic type. If we consider that SK have pulsed stimulations to hyperproliferate or to accumulate, we can admit that all SKs evolve from paucicellular smooth lesions of the reticulate-acanthotic type to pluricellular thickened SK of the acantho-hyperkeratotic type. These paucicellular smooth lesions arise from macular SK, considered by some a solar lentigo. No clonal SKs were detected in our study and their probable rarity does not enable us to hypothesize a relationship between the clinical and histological picture of this subtype.
This is important in clinical trials with topically applied substances. Indeed clinical evaluation of lesions enables an accurate determination of the histological type, and subsequently an estimate of the penetrability of the substance (especially if lipophility is an issue because of the thickness of the Stratum corneum) in the lesion.
As a conclusion, the diagnosis of SK can be made on clinical grounds with the help of dermoscopy. Nevertheless, in case of diagnostic doubt, with a melanocytic lesion, histological shave biopsy should be done. Histology mostly helps but diagnosis of SK can be impossible if the location of the shaved lesion is unknown. Also in most cases, a guess of the histological type on clinical grounds is straightforward.
This advice is for informational purposes only and does not replace therapeutic judgement done by a skin doctor.
Contributors:
Dr Christophe HSU – dermatologist. Geneva, Switzerland