Clinical Features (For Professionals)
Dr Christophe HSU – dermatologist. Geneva, Switzerland
Clinical Presentation
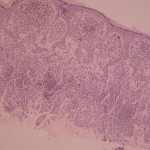
Usually, the diagnosis is straightforward. Histology is needed in doubtful cases.
{Pierson, 2003}SKs have many ways of presenting, they can appear as macules, papules or plaques which are normally sharply demarcated from the surrounding normal skin. They are generally brown in colour but can be lighter or on the contrary be more pigmented. When traumatized or when a horn cyst ruptures, the lesions can provoke pruritus and show an inflammatory aspect with crusting {Pierson, 2003} and an erythematous halo around the base of the lesion {Habif, 2001}is sometimes seen.
With the passing of time, the macular SKs which are considered as senile (solar) lentigos become verrucous, polyploid and pedunculated, and with progressing development have an increasing stuck on appearance.
Most of the lesions have a diameter between 5 mm and 1 cm even though rarely some SKs, called giant SKs, exceed 5 cm{Kao, 2000}
{Pierson, 2003}Keratotic plugging with follicular prominence contributes to a stippled or velvety surface and imbues a “stuck-on” appearance.
SK is distributed on follicular skin (see etiology follicular) exclusively. It is therefore not found on the glabrous skin of the palms and soles, as well as the mucous membranes. The trunk, head and neck are the most commonly involved areas {Pierson, 2003}.
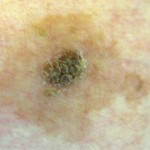
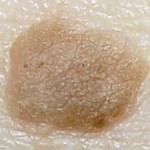
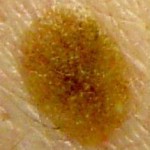
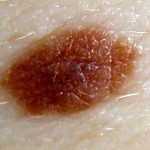
Different clinical presentations of SK. SK can be lightly or darkly pigmented, have a smooth or rough surface; be isolated or multiple. But all tend to be clinically well delineated and have a stuck on appearance.
Multiple SK tend to be distributed on the back of the trunk in a Christmas tree pattern. Our proposal of theory for that distribution is that seborrheic keratosis tend to be flat on the dermo-epidermal junction (see histology). This means that the lesions are found more predominantly when skin folds (preferably deep) are absent. With the passing of time, the skin tends to become more lax and starts falling down, which is what we can see on the back of the trunk(see right figure below). Thus the skin is characterized by alterations of wrinkled and flat skin, which is the area where seborrheic keratosis tend to develop.
Multiple Seborrheic Keratosis on the trunk tend to be distributed in a Christmas Tree pattern. The figure on the right (without lesions) is to help explain the distribution of multiple SKs.
IFK – a histological subtype of irritated SK – presents as an isolated {Degos, 1968; Mehregan, 1964} keratotic papule, having a diameter of 0,3 cm to 1 cm located in 85% on the face (cheeks, upper lip, eyelids), on the rest of the head, the neck and any follicular region. Lesions regress occasionally, but tend to remain persistant. IFK sometimes appear inflamed and are then accompanied by pruritus.
Differential Diagnosis on clinical presentation {Pierson, 2003 #360}
There is usually little diagnostic difficulty when the lesions are numerous. The differential diagnosis is as follows, with the region of predilection of the lesions and remarks:
A. Acrochordon (Skin tags)
localisation
– neck
– eyebrows
– armpits
– inguinal folds
– inframammary folds
(SKs localised here tend to be acanthotic, little keratosis being present. They aren’t pediculated.)
B. Verruca vulgaris
localisation
– legs
– hands and fingers
(Contains Human papilloma virus (HPV))
Histologically different: koilocytosis, parakeratosis, hypergranulosis, dilated capillaries are present.
C. Condyloma accuminata
localisation
– genital region
(Contains HPV)
Histologically different: koilocytosis, parakeratosis, hypergranulosis, dilated capillaries are present
D. Acrokeratosis verruciformis
E. Tumour of the follicular infundibulum
localisation:
– head
– neck
(These tumours are rare and present clinically as a unique papule on people of middle or old age.)
Histologically, there is a plate-like proliferation of pale, basaloid keratinocytes. The proliferation reunites the follicules with the adjacent rete ridges. SKs on the contrary, even if the gross aspect can be confused, do not show a plate-like proliferation.
F. Bowen’s disease (BD) and squamous cell carcinomas (SCC)
Pigmented BD can have a red-brown colour and be clinically indistinguishable from irritated SKs.
A biopsy is necessary in case of diagnostic doubt.
Histologically:
– irritated SKs are often diagnosed as malignant because of cellular atypia (see histology).
– BD and SCC show nuclear shrinking, abundant mitoses and parakeratosis. There is in contrast with SK no abrupt transition with the surrounding epithelium.
– Even though squamous cell carcinomas and SKs contain squamous eddies, the former do not contain squamous eddies in the dermis.
Prospective studies have examined systematically all lesions clinically identified as SKs. In some cases, epithelial cancers {Kwittken, 1981; Mikhail, 1982; Sloan, 1993; Yap, 1997} have been found. In another prospective study, Maize and al (1995) showed that nonmelanoma malignancies (all squamous cell carcinomas) amounted to 4,6 % (5 out of 106) of all specimens.
G. Solar lentigo
Localisation: – in photoexposed areas, mainly on the face {Stolz, 2002}.
Look like macular SK.
Histologically: no hyperkeratosis
Solar lentigo are considered by some as a cause of reticulate SK (Mehregan 1976)
H. Nevocelullar naevus
The differentiation is most difficult when the SK is of acanthotic histological type and that it doesn’t have a stuck on appearance.
Histological examination resolves the problem.
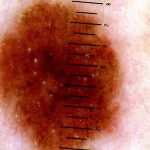
This lesion was thought to be a seborrheic keratosis but histology revealed a naevocellular naevus. What should have aroused doubt is that the lesion did not have a stuck-on appearance. The presence of milia-like cysts shows that this sign alone is not specific of SK.
I. Melanoma
Clinical evaluation of pigmented lesions, and a clinically based diagnosis of SK is sometimes erroneous, with all the potentially grave consequences of missing a malignant melanoma. The most striking example of melanoma simulating SK comes from a study by Blessing {Blessing, 1993}. In a retrospective analysis of 20 patients diagnosed with melanoma, half of he lesions had clinically been diagnosed as benign lesions (papillomas, SK)s. (10% of histology reports were that of benign lesions)
Thomas et al{Thomas, 2004} examined a 70 year old patient of Italian descent. Clinically, the lesion had a stuck-on appearance and horn cysts in the right temporal region. The lesion measured 7 mm by 4 mm and had grown progressively for 2 years. The shave was done because the patient had noted a change in appearance. The histological analysis was a superficial spreading melanoma!
Thomas et al {Thomas, 2004}acknowledged that a clinical differentiation between pigmented lesions of melanocytic or non melanocytic origin is a useful first step, but that the clinician must not ignore the potential for spinous cell carcinomas, basal cell carcinomas or even {Kwittken, 1981; Yap, 1997; Sloan, 1993; Mikhail, 1982} melanomas within the lesion. Verrucous melanoms, as an example, are easily confused with SKs({Blessing, 1993; Steiner, 1988; Schwartz, 1980}.
Thomas et al {Thomas, 2004}concluded that a clinical diagnosis isn’t reliable; because a SK can have many different colours within it; that their dermoscopic features and that the signs that evocate a malignant melanocytic lesion (ABCD rule, change in colour, pain, irritation, pruritus, ulceration, bleeding and crust formation) must not be overlooked.
J. Melanoacanthoma
A sometimes considered type of SK, is often confused clinically with malignant melanoma, particularly so when it is located in oral mucosa {Blessing, 1993}. It appears after trauma in affects people aged 20 to 50 of black colour, more often women. Histologically, abundant dendritic melanocytes are seen as well as acanthosis of the buccal mucosa {Blessing, 1993}.
K. Basal cell carcinoma
Even though pigmented basal cell carcinoma can mimic SK, they are sometimes hidden behind a SK. Basal cell carcinoma is the most frequently associated cancer with SK {Cascajo, 1996; Rao, 1994} {Zabel, 2000}. Sloan et al (1993){Sloan, 1993}reviewed 4310 cases clinically diagnosed as SK. A histological examination revealed 60 (1,4%) of these cases as basal cell carcinomas. But because of the high prevalence of these lesions {Zabel, 2000}, a “collision” theory has emerged suggesting that these very prevalent lesions develop independantly juxtaposing on each other.
This advice is for informational purposes only and does not replace therapeutic judgement done by a skin doctor
Contributors:
Dr Christophe HSU – dermatologist. Geneva, Switzerland