Drug Eruptions in the Skin (toxiderma) (For Professionals)
Our skin reflects our health. Do you know that our skin also reacts to the drugs that we use?
- A drug reaction may mimic any type of skin disease and may present with rashes, swelling, redness, itching and pain. They can be bullous, pustular, urticarial or papulosquamous. However, the etiology (cause) is a certain drug that we take in.
- So, how do we know that what we are having is not a simple skin disease but a drug reaction? First of all, a drug induced reaction should be suspected when a person develops skin lesions after taking some medications. These medications may be in the form of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, acetaminophen, ibuprofen; or antibiotics such as penicillins, drugs for chemotherapy, drugs for convulsions, drugs for psychiatric disorders and any other drug.
- The mechanisms why these drugs cause the said skin lesions are two-fold: they may either be triggered by immune response reactions or non-immune response reactions.
- Immune response reactions may either be of four types:
- Type I is an immunoglobulin E (IgE)–dependent reaction, which results in rashes (urticarial in nature), swelling, and anaphylaxis or allergic reaction. The best example of this type of reaction would be the reaction observed in some patients after insulin (or any other protein based) injection.
- Type II is an cytotoxic reaction, which results in redness of the skin and small bruises called purpura. The example of this reaction would be the reaction of some patients to antibiotics such as penicillins, cephalosporins, sulfonamides, and rifampicin.
- Type III is an immune complex reaction, which results in inflammation of the blood vessels called vasculitis, serum sickness, and manifests as urticaria or itching and rashes. The example would be the drug reaction associated with quinine an antimalarial drug, salicylates for pain, chlorpromazine for psychiatric disorders, and sulfonamides which are antibiotics with sulfur components.
- Type IV is a delayed-type reaction with hypersensitivity, which results in contact dermatitis manifested as peeling, rashes and redness, pain and itching. Examples of these drugs reactions are the ones encountered secondary to neomycin and sulfonamides, which may also cause toxic epidermal necrolysis (TEN)*. The latter lead to painful red lesions which involves the mucosal tissue and the skin can slough off (Nikolsky’s sign) These drugs reactions appear 7-20 days after the medication is started, they may involve blood or tissue reactions, and they may recur if the drugs are administered.
Toxic Epidermal Necrolysis (TEN, Lyell Syndrome): Clinical Picture (1)
Toxic Epidermal Necrolysis (TEN, Lyell Syndrome): Clinical picture with positive Nikolsky sign: slight rubbing of the skin results in exfoliation of the outermost layer”
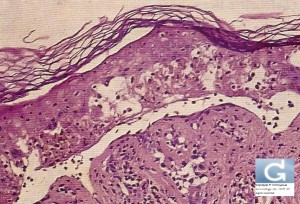
Toxic Epidermal Necrolysis (TEN, Lyell Syndrome): Histology of the skin shows necrotic keratinocytes with full-thickness epithelial necrosis and detachment
*TEN may also be called Lyell syndrome
Milder forms of TEN are called Stevens-Johnson Syndrome (SJS)
-SJS is defined as lesions occupying less than 10% of the Body Surface Area (BSA)
-Lyell syndrome is defined when the body surface involved is more than 30%
-SJS/Lyell overlap is defined as a BSA between 10 and 30%.
- The next type of drug reactions is non immune related. They are related to adverse effects, cell reactions in the blood to the drug components, or intolerance to the drug…
- An example would be the Jarisch-Herxheimer reaction, which is an inflammatory response to antibiotic treatment for certain diseases (Syphilis is the classical example)((although some non-antibiotic treatments can produce the reaction). A Herxheimer reaction feels like a worsening of illness symptoms and can include fever, sweating and chills, rapid heart rate or palpitations, shortness of breath, muscle and joint aches and pains, headache, brain fog, insomnia, swollen glands, ringing in the ears, sinusitis, itching and digestive issues.
- Another example of the non immune related drug reaction would be a blue-gray discoloration of skin and nails observed with substances containing silver (E.g. the use of silver nitrate nasal sprays. This is termed by doctors as “argyria”. Other reactions belonging to this category would be hair loss with cyclophosphamide, a chemotherapy drug, urticaria with aspirin (histamine release by mast cells), and rashes (maculo-papular) due to ampicillin (an antibiotic). Again, these do not involve immune response elements such as the formation of antibodies to the drug component in the body.
- It is said that worldwide, drug eruptions occur in approximately 2-3% of inpatients. Most drug eruptions are mild, self-limited, and usually resolve after the drug has been discontinued. Death may occur in approximately 1 in 1000 hospital patients. Also, adverse skin reactions to drugs are more common in women than in men and that elderly patients have an increased risk of adverse drug reactions.
So what do I need to do if I get a drug reaction?
- The first step is to consult your doctor, who will review your complete medication list, including over-the-counter medicines and supplements. The doctor is also going to ask you about any history of previous adverse reactions to drugs or foods. Infections and other diseases can also predispose you to a drug reaction.
- Next, the doctor is going to examine your skin lesions. It is more likely to be a drug reaction if you have a some of the following (in addition to a history of drug intake):
- Signs: sore throat, difficulty in urinating, arthritis, abdominal pain, general body malaise, breathing difficulties (dyspnoea)
- Symptoms: mouth or other mucous membrane sores, blisters, a positive Nikolsky sign (epidermis sloughs with finger pressure; indicates serious eruption that may constitute a medical emergency), tongue swelling, redness, palpable bruises, skin discoloration on the legs or any part of the body, enlarged lymph nodes, high fever, a decreased blood pressure, pus filled growths on the upper part of the body, tenderness, edema, erythema of all palms and soles, widespread inflammation of the skin, enlargement of the liver and spleen, increase in white blood cell count, increase of the number of eosinophils in the blood, decrease in red blood cell and hemoglobin count
- The drugs that you have to watch out for are the following: amoxicillin (Augmentin…), trimethoprim sulfamethoxazole (Bactrim…), ampicillin, penicillins, cephalosporins, quinidine, diuretiques (hydrochlorothiazide, furosemide)), heparins, sulfasalazine, dapsone, anticonvulsants (Valproic Acid…), quinolones, ketoconazole, clindamycin, primaquine, tetracycline, pentamidine, NSAIDs, erythromycin, zidovudine, allopurinol, Bumetanide, captopril, penicillamine, piroxicam. But again, any drug can be implicated.
- History and physical examination are often sufficient for diagnosing mild asymptomatic eruptions. Severe or persistent eruptions may require further tests like biopsy, CBC, serum chemistry tests, antibody and/or immunoserology tests, cultures, urinalysis, stool guaiac tests, chest radiography…
- The most important thing in the event of a drug eruption is to stop the drug immediately. Therapy for most drug eruptions is mainly supportive in nature. Antihistamines and steroids may be given. More complex treatments may be given by your doctor according to the diagnosis (e.g. Intravenous Immunoglobulins in the case of Lyell Syndrome).